Information for Physicians about Wound Care and Vascular Care
Clinical Burden of Amputation
•PVD incidence estimated at 10-12 million and growing by 1 million each year
•1-2 million people suffering from critical limb ischemia
–25% 1-year mortality rate
–60% 3-year mortality rate
•150,000 amputations still performed each year.
•50% of patients are treated with primary amputation
•51%-73%of amputations are performed without angiographic evaluation
•70-71% of patients have amputation and never have any revascularization
•One year mortality after CLI diagnosis and amputation is 40%
Following an initial LEA due to dysvascular causes:
- 27% will have 1 or more re-amputation(s) within 1 year
- 40% progressed to a higher level of limb loss within a year of an initial toe, foot, or ankle amputation
- This rate rises to 62% among those with comorbid DM
- 55% of those with PAD will get the other limb amputated within 2-3 years
What is the Multidisciplinary PULSE Program?
•Multidisciplinary approach to amputation prevention where the patient is at the center of the care with a team of specialist working in unison
•Focus is to optimize perfusion for targeted wound healing:
•CLI Specialist- Interventional Cardiologist or Vascular Surgeon, Interventional Radiologist
• Manage all care with Wound care team to expedite wound healing and prevent major amputations.
•Amputation Prevention coordinator/navigator is on the team to lead coordination of care to ensure all aspect of care are cohesive, efficient and focused on optimal treatment for limb salvage.
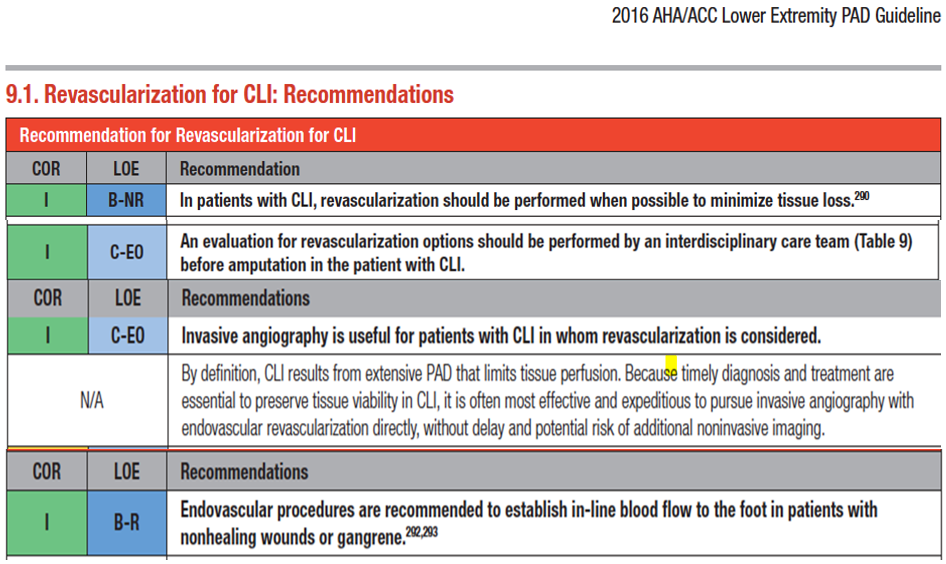
Consensus Recommendations by CLI Global Society :
Managing Critical Limb Ischemia (CLI)
Step 1: Patient presenting with risk factors ( diabetes, CKD, smoking, age >50)
Assess for below:
•Lack of palpable pulses (note: pulses appreciated with doppler do not exclude possibility of severe disease)
•Lower extremity ischemic changes (ie: pain, cramps, discomfort, color or temperature changes)
•Pain at rest or disturbs sleep (pain cramps , with feet up or down)
•Wounds or gangrene of the toe, foot or ankle lower leg
Step 2 :Action to address CLI
- Consult Limb Preservation Specialist immediately (must be immediate due to seriousness of problem)
- Facilitate diagnostic studies as directed by Limb Preservation Specialist
- This may include, but not limited to :
•Arterial dopplers-ultrasound
•TCPO2
•ABIs
•Angiogram
•Peripheral intervention
•Foot X rays
•MRI
(it is best to allow specialist to order these as they can expedite)
*Vascular specialist, Podiatric specialist and or Wound care specialist)
PULSE Team... we are the Limb Preservation Specialists!!
PULSE Team will take care of all work up manage coordinated care with all specialists:
Podiatry, Vascular, Infectious Disease
We have a team of physicians committed to manage patients urgently with all diagnostics, IV antibiotics and all workup done through our team.
All Urgently within 24-48 hours with ONE referral
Hispanics are at higher risk:
•Minorites had both a higher incidence and proportion of diabetes-related LOWER EXTREMITY AMPUTATION (LEA), compared with non-Hispanic whites.”
•Mexican Americans had MORE diabetes-related amputation, 85.95% than blacks or non-Hispanic whites 74.7% & 56.3% respectively
•The risks for major amputation were significantly higher… in Hispanic patients with Diabetic Foot Infections (DFIs) compared to White patients2
Disparities in Treatment of CLI Patients:
- Primary Care Doctors are overwhelmed and extremely busy leading to delays in referral process
- Delays in referral for vascular evaluation due to long waits for appointments
- Delays in referral for proper wound management due to long waits for appointments
- Poor communication among the various specialists
- Poor follow up and readmissions related to non compliance
- Too many appointments and traveling to different physicians leads to poor compliance
ALL THESE LEAD TO FRAGMENTED CARE AND UNECESSARY AMPUTATIONS!
THE SOLUTION:
Multidisciplinary approach to amputation prevention where the patient is at the center of the care with a team of specialist working in unison
The Process:
•Call the Hotline: 915-243-FOOT (3668)
•PULSE Team will triage patient in hospital and outpatient to manage care efficiently and optimize wound healing
•All efforts are made to manage care outpatient if possible in an efficient coordinated manner, if inpt all efforts are made to revascularize first and coordinate care
•We will help manage in the hospital and handle the direct admission of the patient if needed with all consults and orders in place early to expedite care
•We will continue to manage the patient in post acute care- LTAC, SNF, Home health care
•Once DC we manage outpatient…We schedule patient to be seen in PULSE clinic next day or within the week depending on acuity. (If pt. stable for DC we can manage outpatient)
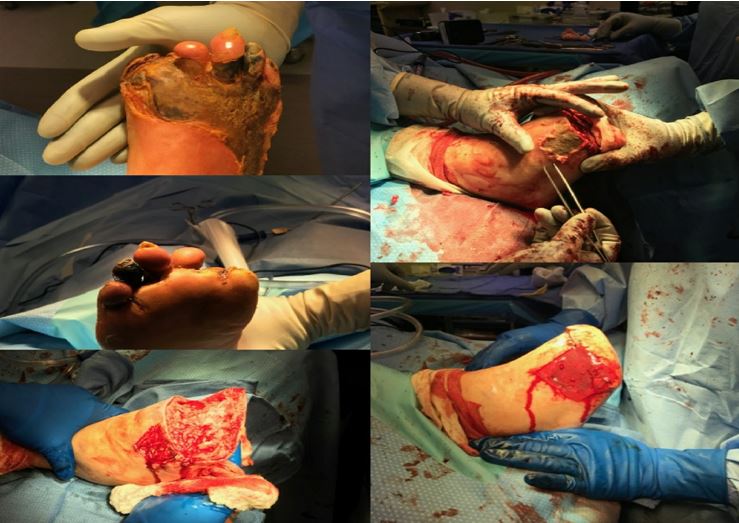
Surgical Approach:
- Patient with an extensive gangrenous infection to his left forefoot.
- Left foot transmetatarsal amputation performed
- Plantar Tissue Flap
- Applied a cross linked bovine tendon collagen, bilayer wound matrix allograft to the soft tissue defect proximal to the amputation site.
- TMA site healed uneventfully
- Proximal wound healed by secondary intention
Care Coordination
- Follow up through rehab admission after discharge from hospital with follow up doppler studies at 1 month
- Coordination with Home Health upon discharge for wound care in wound care center and daily in home health and surveillance of wounds and vascular
- Planned debridements and vascular surveillance follow ups with Dr Raja every 3 months.
- CHF hospitalization – performed vascular eval and doppler studies during this visit to evaluate vascular status
- Targeted referral to Dr. Szeyko to manage venous stasis wound
The Functional Foot
•Healed after 6 months
•Ambulating with orthotic shoe
•Close surveillance
•Team approach to Limb Salvage
AMP 2020 Virtual | Different Types of Infrainguinal Calcification
AMP 2020 Virtual | Time Consumption for Performing CLI Interventions
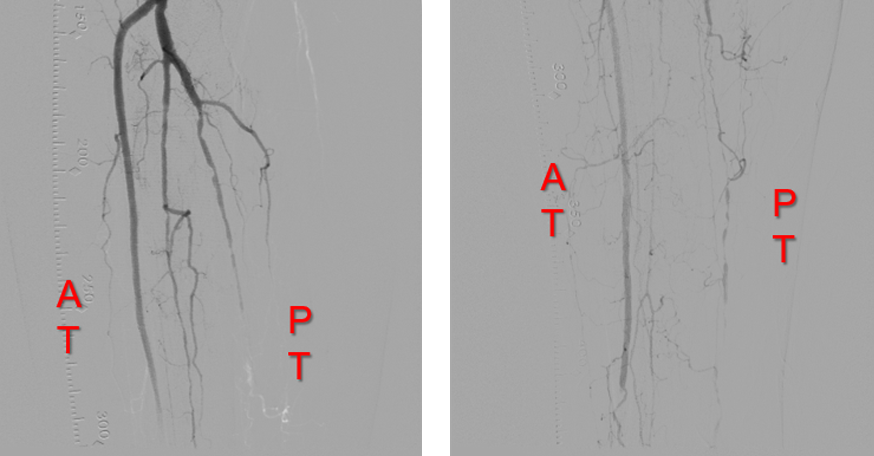
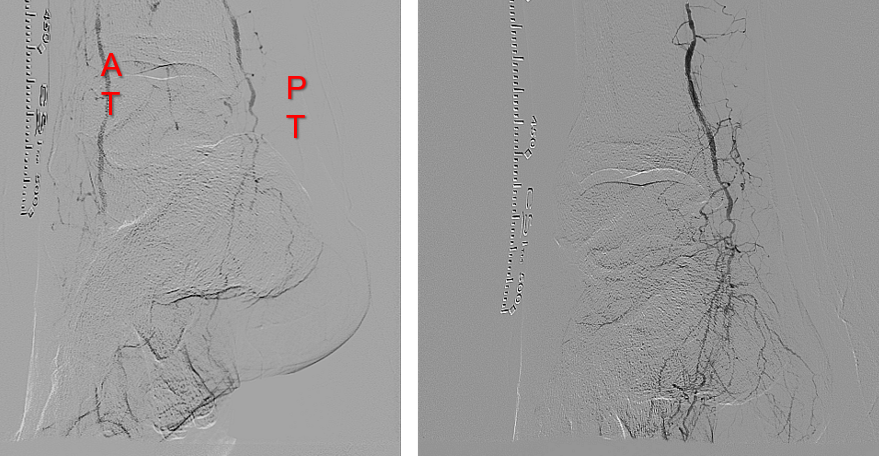
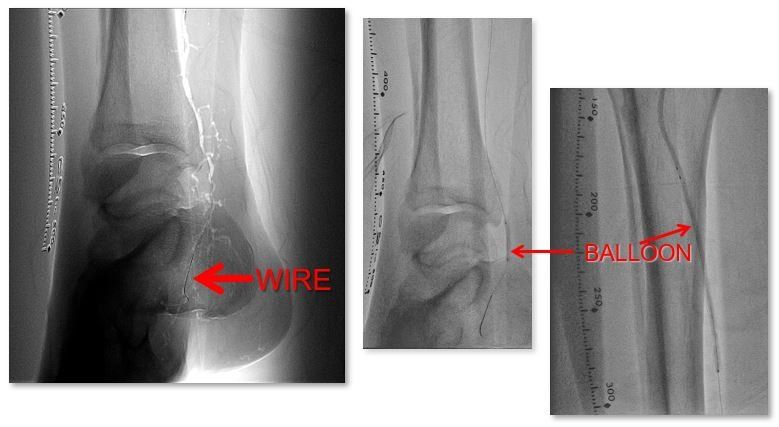
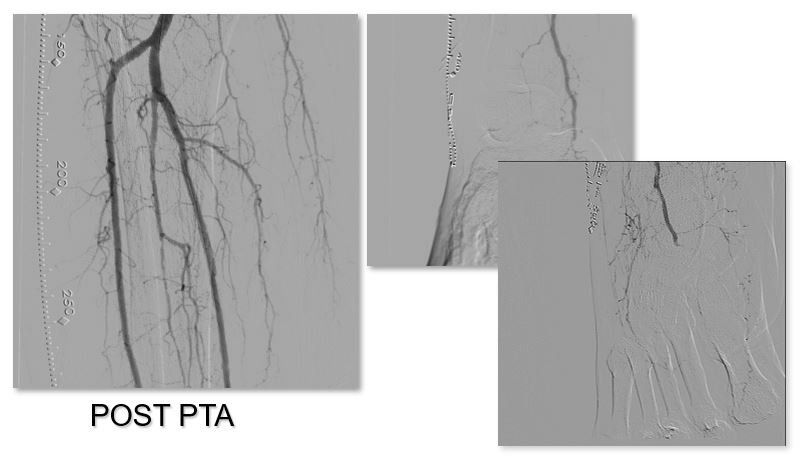
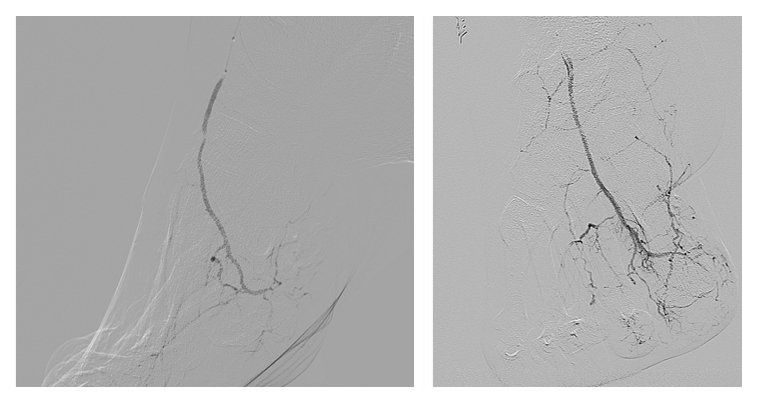
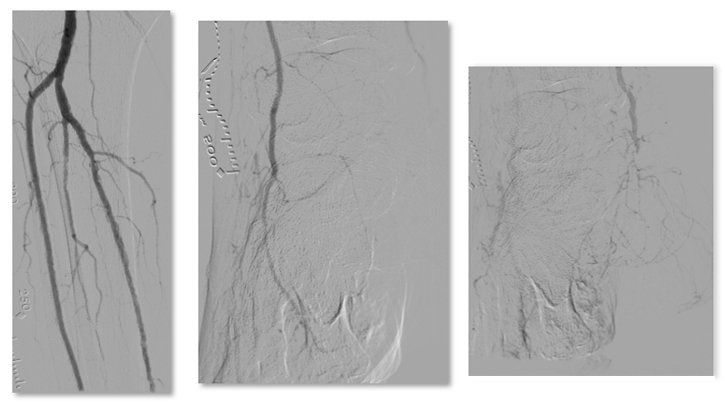
LIVE Case Dr Raja
Orbital Atherectomy
Complex SFA CTO Crossing and Treatment
CONTACT INFORMATION
PHONE:
ADDRESS:
4301 N. Mesa Ste . 100
El Paso Texas 79902
2311 N Oregon St
5th Floor El Paso, TX 79902
OUR LOCATION